Cluster: The Suicide Headache
/Jerry Rodriguez’s story:
I was 41 years old with a successful auto body repair shop, a wife I loved and two great kids. Why did I drive to the Coronado Bridge with a plan to jump? What could be so bad that I would leave my wife a widow and my children without a father? I was in grips of a cluster headache cycle, and I just couldn’t live with it anymore. The pain was unimaginable. The only way I knew to end the headaches was to end…me. Thankfully there was heavy traffic on the I-5 that day. By the time I reached the exit for the bridge, my headache was gone, and rational thought had returned.
My headaches had started five years before with my first cluster cycle. I had 2 to 3 attacks a day at random times without any obvious trigger, and one attack always, always would wake me up from a sound sleep at 2:00 AM every night. Each attack was the same. Without warning, I would get excruciating pain around my left eye. Like a knife was plunged into my eye and then twisted. My eye turned red and watered like a hose. My left nostril became stopped up, and my eyelid would droop. This pain was unbearable. I once smashed my finger in a car door. This cluster headache pain was like that finger-in-the-car-door pain, but it lasted for one hour exactly. I paced, I banged my head on the wall. I even tried smearing Vick’s VapoRub in my eye hoping that new pain would offset the cluster pain. No luck.
Brain MRIs were always normal. Eye exams were normal. Scans of my sinuses were negative. No one could give me an explanation for why this was happening. Some doctors called it migraine, others said it was sinusitis. The only medication that ever helped was injectable sumatriptan, and my insurance company covered 6 injections a month. With 3 attacks a day, the prescription didn’t last long.
After a couple of months, the attacks became less frequent and didn’t hurt as much. Eventually they stopped altogether. Almost a year went by with no attacks, and I was so thankful it was over. But then in the fall, another cycle began just like the first one. This pattern of cycle-on, cycle-off persisted for over five years. I suffered a lot. And my family suffered with me.
In the end, all it took was 30 minutes with a specialist whose office was less than a mile from my shop. Cluster, he told me. You’ve got cluster. That was it. A diagnosis. Treatment, and thank God, no more suffering.
Mr. Rodriguez’s story is illustrative of cluster’s malevolence. Many healthcare providers and those afflicted with the disorder often refer to cluster as “the King of Headaches”. Its more somber and unfortunately well-deserved nickname is “The Suicide Headache”.
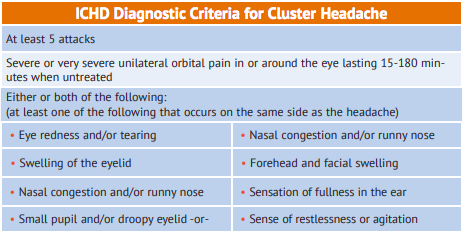
The current ICHD (International Classification of Headache Disorders) criteria for diagnosis of cluster headache are listed in the table below, and the most specific of these criteria involves the duration of an individual cluster attack. Other primary headache disorders - notably migraine - may be “side-locked” (ie, invariably occur on the same side of the head), severe in intensity, centered primarily in or behind the eye and even accompanied by eye tearing, a runny or stopped-up nostril and eyelid drooping, but cluster is notable for its relatively short duration. By definition, cluster lasts from 15 minutes to three hours (and usually an hour or less), whereas untreated migraine typically lasts for hours to days. Patients presenting to a headache clinic declaring that they have “cluster” and reporting that their headache attacks last up to days may have migraine with cluster features, but they do not have cluster, per se. It’s an important distinction to make; while certain therapies may be effective for both cluster and migraine, many are much more effective for one disorder than the other.
The demography of cluster also is distinct from that of migraine. As many as 12% of Americans (40 million) have clinically active migraine; in contrast, the one year prevalence of cluster is much less than 1%. While migraine is roughly 3 times more prevalent in females than in the males, cluster is approximately 4 times more common in males. Cluster tends to begin later in life than migraine, and cluster patients report a family history of cluster less often than migraine patients report a family history positive for migraine. Migraine clearly appears to be genetic in origin, but whatever genetic component cluster may have has not been clearly identified. Cigarette smoking has been linked to cluster, but far from all cluster patients have been smokers in the past or actively smoke.
Just as migraine often is misdiagnosed as cluster, cluster frequently is misidentified. Attacks of cluster head pain may be attributed to trigeminal neuralgia, a dental abnormality, a primary eye disorder (e.g., glaucoma), temporomandibular joint disease or sinus disease, leading to unnecessary (and often invasive) testing, prescription of inappropriate medication and procedures that range from dental extraction to brain surgery. As if the the suffering and expense associated with receiving an inaccurate diagnosis and treatment plan were not bad enough, such mismanagement is easily avoidable. As with migraine, cluster headache is a diagnosis made largely on the basis of the patient’s history, and so vivid, “technicolor” and specific is the typical cluster history that misdiagnosis should be rare. If you or someone close to you may have cluster, seek care from a healthcare provider experienced in the diagnosis and management of headache.
Cluster is most definitely treatable. A short course of high-dose oral steroid can be highly effective in ending a cluster cycle, as can the antihypertensive drug verapamil or a particular type of easily performed nerve block (suboccipital nerve block). Recent research suggests that the CGRP antagonists also may prevent episodic cluster. Acute attacks of cluster tend to be exquisitely sensitive to treatment with injectable sumatriptan, and for those patients who fail to respond to that drug or in whom it is contraindicated, inhalation of high flow oxygen delivered via a rebreather mask can terminate the agonizing pain.
While cluster is uncommon relative to migraine, it is far from rare. Whatever its relative frequency, the pain of cluster headache is notoriously severe - to the point of being life-threatening - and cluster patients require and deserve an accurate diagnosis and appropriate treatment.