Occipital Nerve Blocks: Miracle therapy or glorified placebo?
/Over the past two decades this author has performed occipital nerve blocks (ONBs) over 10,000 times for the treatment of headache. The patients receiving those blocks have been a varied lot, but most have had “cervicogenic headache“, a term surprisingly unpopular with a number of headache specialists but nevertheless adequate for its descriptive value if not its specificity.
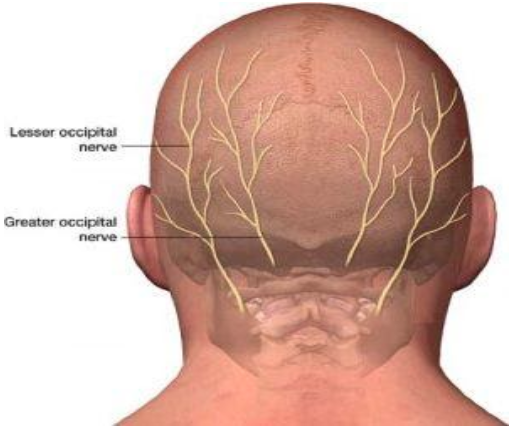
“Cervicogenic“ means simply “born of the neck“, and patients with cervicogenic headache experience head pain that originates from the upper neck or skull base and radiates anteriorly towards the front of the head. Cervicogenic headaches often result from abnormal hypersensitivity of the occipital nerves, two nerves - one on each side - which arise from nerve roots that depart the upper portion of the spinal cord and, like the tributaries of a river, join together to form the nerves themselves. The main trunk of the occipital nerve travels up over the skull base at the back of one’s head, and divides into two major branches (the greater and lesser occipital nerves) which supply sensation to large portions of the scalp.
The same nerve roots that contribute to the occipital nerve also send fibers that connect with a substation for transmission of head pain signal that resides within the lower portion of the brain stem. That substation is called the trigeminal nucleus caudalis (TNC). The TNC is an important part of the circuitry that generates the pain of migraine headache and, quite likely, the pain of headache generally. The headache relief provided by the triptans (e.g., sumatriptan; Imitrex) may in part result from their stimulation of "off-switch" receptors located within the TNC that block the transmission of head pain signaling.
As a substitute for “cervicogenic headache“ one could substitute “occipital neuralgia“, a term which in the broadest sense implies pain experienced over the posterior portion of the head consequent to a process compressing, inflaming or otherwise irritating the occipital nerves. “Classical“ occipital neuralgia tends to resemble its facial pain equivalent, trigeminal neuralgia (tic douloureux), with brief, repetitive paroxysms of pain often described as “shooting“ or “like electricity“ and at times triggered by pressing upon the nerve involved. Far more frequently, however, clinicians encounter “plain old occipital neuralgia”, a much more persistent and pervasive pain that arises from the skull base and extends forward. At times the pain associated with this type of occipital neuralgia may radiate forward to the eye on the same side.
Cervicogenic headache (or “plain old occipital neuralgia“, if you prefer) may occur consequent to an obvious precipitant. For example, the “whiplash“ neck injury that one may suffer from being rear-ended while driving often produces cervicogenic headache in addition to neck pain and stiffness. Many times, however, there is no obvious cause, and in many cases cervicogenic headaches arise in migraineurs whose migraine has taken a turn for the chronic.
An ONB involves an injection of a local anesthetic into the area immediately around the main trunk of the occipital nerve, its two main branches, or both. Many clinicians who perform these blocks will add a steroid anti-inflammatory medication to the local anesthetic, but it remains controversial whether the steroid provides any additional benefit over the local anesthetic alone. The blocks may be performed via a suboccipital approach (with insertion of the needle just under the skull base so as to reach the main trunk of the nerve before its first division), or it may be performed via an occipital approach, with injections made on the scalp in the regions of the greater and lesser occipital nerves.
The hallmark of a successful ONB is the rapid onset of significant pain relief, often occurring within 15 minutes of the block. It is more or less a given that absence of improvement over the first 24 hours following the block indicates the procedure was a failure. Delayed improvement is unusual. In responders the improvement is so rapid that headache subspecialists often use ONBs as a way to treat a patient with acute migraine headache, especially when the headache has persisted for a few days or more.
If there is relief, how long will the relief last? A good question and the answer is: anywhere from a day up to forever…or anything in between those two extremes. As a rule of thumb, the duration of relief received from one’s first block predicts what will be the duration of relief if additional blocks are performed. In patients with chronic migraine possessing a prominent cervicogenic component, substantial headache relief may persist for a period of months before "wearing-off", and in that way, the therapeutic response resembles what is seen with serial Botox injection therapy or use of the new anti-CGRP monoclonal antibodies
Are the blocks safe? In the hands of an experienced provider, an occipital nerve block is a simple procedure that requires only a minute or so to perform and can be administered in the course of a routine clinic visit. On occasion patients almost immediately develop a vasovagal response characterized by nausea and lightheadedness. The treatment is pretty simple: the provider will have the patient lie down and elevate his/her legs, offer the patient some water, and wait until the reaction passes (which it does within a few minutes). After receiving the blocks a patient may leave the clinic and return to usual routine activities… hopefully headache-free and consequently well-pleased.
Do occipital nerve blocks actually "work", or is the reduction in headache simply a placebo response? Because it is so difficult to conduct a meaningful clinical research study that would involve a comparison of occipital nerve blocks and placebo, the evidence to support the blocks’ "true" effectiveness is derived chiefly from observational studies involving large numbers of patients so treated and from routine clinical experience. In one "open-label" trial conducted by the author and his colleagues and published in Headache, the journal of the American Headache Society, 60% of 150 consecutive patients with cervicogenic chronic migraine who were treated with ONBs experienced significant headache relief that persisted for at least 1 month following the procedure. As for experience in routine clinical practice, any provider who has seen a sufficient number of headache patients and performed a sufficient number of occipital nerve blocks will tell you that the clinical response is so stereotyped that it would be very difficult to attribute that response to placebo only.
Sadly, as is the case with many migraine therapies, insurers often resist providing authorization for ONBs. At the other end of the spectrum, there are surgeons - many of whom are highly reputable and clearly well-intentioned - who perform occipital nerve decompression surgery at a dollar-cost that reaches into 5 figures. Somewhere in between the North Pole of "we will not authorize this procedure" and the South Pole of occipital nerve decompression surgery lie therapies such as occipital nerve stimulators and a more invasive block of the occipital nerves that involves radiofrequency ablation (often known by the acronym RFA).
Suffice it to say that ONBs may represent an excellent treatment option for patients plagued by cervicogenic chronic migraine or cervicogenic headache of other causes that have resisted treatment with medications intended for headache prevention. If you are a migraineur with chronic cervicogenic migraine and you wish to pursue this option, seek out a headache subspecialist who has extensive experience with ONB. The American Headache Society’s patient website can be an enormous help in locating such a provider.